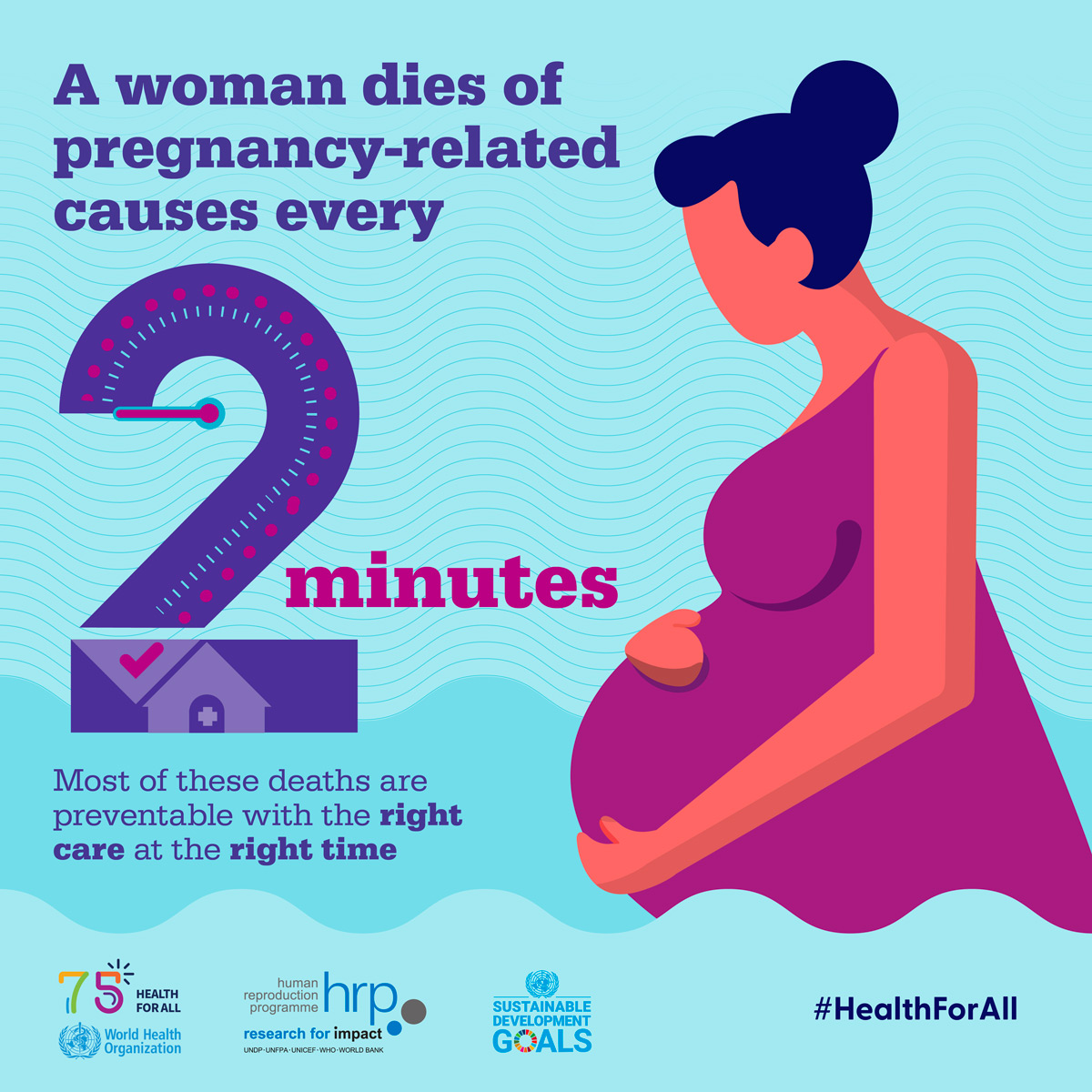
Maternal mortality is a pressing public health issue that has been on the rise in the United States, alarming both healthcare professionals and policy makers alike. Recent studies reveal that more than 80 percent of pregnancy-related deaths are preventable, highlighting a critical maternal health crisis. Contributing factors include inadequate prenatal care and poor postpartum care, which disproportionately affect racial minorities, magnifying racial disparities in maternal health. The California maternal mortality rates illustrate a stark contrast, suggesting that effective policies can significantly reduce preventable pregnancy deaths. Urgent reforms in healthcare systems are necessary to bridge the gaps and ensure that every mother receives the support she desperately needs.
The phenomenon of pregnancy-related deaths has come to be recognized as a serious health concern, often referred to in broader terms such as maternal morbidity and mortality rates. This crisis, characterized by avoidable fatalities during and after childbirth, underscores the need for improved access to comprehensive maternal healthcare services. The disparities faced by various demographics, particularly along racial lines, raise significant questions about equity in health outcomes. Addressing postpartum health and the broader impacts of chronic diseases can further enhance the quality of maternal care across different states. Emphasizing community-based solutions may help tackle the issues surrounding preventable maternal deaths, fostering a healthier environment for mothers and their children.
Understanding Maternal Mortality in the U.S.
The alarming rate of maternal mortality in the United States highlights a significant public health crisis. With a maternal mortality rate higher than any other high-income country, over 80% of these deaths are classified as preventable. Despite advancements in medical technologies and prenatal care, systemic issues continue to plague the healthcare system. For instance, a 2022 report showed that maternal mortality rates increased to 32.6 deaths per 100,000 live births from 25.3 in 2018, illustrating a pressing need to address underlying factors contributing to this health crisis.
Research indicates that disparities exist not only on a national level but also among different racial and ethnic groups. For example, American Indian and Alaska Native women experienced a staggering mortality rate of 106.3 per 100,000 live births, which is nearly four times that of white women. This paints a stark picture of the inequities pervasive within our healthcare system, underlining the urgent need for comprehensive reforms that prioritize equitable healthcare access to combat these troubling statistics.
The Role of Preventable Pregnancy Deaths
Preventable pregnancy deaths remain a heart-wrenching issue as they underscore missed opportunities in maternal healthcare. High rates of preventable deaths highlight significant gaps in prenatal and postpartum care that could otherwise safeguard maternal lives. Healthcare professionals advocate for an overhaul of the current systems to ensure that all women receive the quality and continuity of care they need before, during, and after pregnancy. Investing in better education around risk factors and enhancing access to care can significantly mitigate these preventable risks.
The evidence suggests that better care coordination and patient education can help reduce preventable deaths. Enhanced access to postpartum resources, as well as comprehensive mental health support, can play a vital role in addressing the complexities surrounding maternal health. It is imperative that stakeholders evaluate the current frameworks and implement innovative solutions geared towards improving overall maternal health outcomes.
Postpartum Care: A Critical Component
Postpartum care is often neglected despite being a crucial period for maternal health. Many women are discharged from hospitals within days of giving birth with insufficient support structures in place. Addressing this gap can dramatically lower the rates of maternal mortality, especially since nearly one-third of pregnancy-related deaths occur in the postpartum period. Extending care beyond the traditional six-week postpartum check-up to include regular monitoring and support for a full year after birth can directly impact maternal health quality, reducing risks associated with chronic conditions.
The shift towards recognizing the postpartum period as a continuum rather than a fixed point in time aligns with emerging research advocating for more inclusive healthcare practices. For instance, enhanced support during the awkward transition to motherhood, alongside proactive management of potential complications, can pave the way for healthier outcomes. Policymakers must prioritize developing protocols that ensure thorough follow-ups and sustained healthcare access, thus bridging the gaps caused by the limited definition of postpartum care.
Racial Disparities in Maternal Health Outcomes
Racial disparities in maternal health outcomes spotlight the systemic inequities present within the U.S. healthcare system. The consistent and alarming differences in maternal mortality rates between racial groups demonstrate a need for targeted interventions. The statistics reveal that Black and Indigenous women face vastly higher risks during pregnancy and childbirth, often attributed to factors like systemic racism, socioeconomic status, and access to quality care. Addressing these disparities requires not just healthcare reforms but a societal commitment to dismantling the underlying structural biases that exacerbate these issues.
For meaningful change to occur, healthcare systems must integrate culturally competent care practices that acknowledge and address the specific needs of underrepresented communities. This involves training healthcare providers to better understand the social determinants of health that disproportionately affect these populations. By fostering an environment that values diversity and inclusivity, we can work towards equalizing maternal health outcomes and ultimately reduce the preventable pregnancy deaths that plague certain racial demographics.
California’s Success in Reducing Maternal Mortality
California serves as a benchmark in the fight against maternal mortality, boasting some of the lowest rates in the nation. This success can be attributed to proactive policies and innovative programs aimed at providing comprehensive maternal care. From implementing statewide initiatives like the Maternal Quality Care Collaborative, California has focused on improving healthcare access and fostering collaboration among providers to share best practices. The state’s approach serves as a model for other regions grappling with higher maternal mortality rates.
The stark contrast between California’s achievements and the national average underscores the potential for other states to replicate such success. Challenges remain, as several states continue to struggle with significantly higher rates of maternal mortality. By analyzing California’s data-driven strategies and community engagement efforts, a roadmap emerges for others to follow in refining their maternal health policies. Sustainable change comes from commitment, innovation, and a shared goal to protect the lives of all mothers through quality care.
Improving Maternal Healthcare Infrastructure
Strengthening the maternal healthcare infrastructure is pivotal in addressing the rising maternal mortality rates in the U.S. The current healthcare landscape often fails to provide the necessary support systems, particularly for vulnerable populations and those living in rural or underserved areas. Efforts must focus on creating a seamless continuum of care, ensuring women have access to necessary resources before, during, and after pregnancy. This can involve bolstering healthcare facilities, enhancing transportation services, and investing in telehealth solutions to reach those in remote locations.
Moreover, investing in maternal health infrastructure includes training healthcare providers to recognize and manage the unique challenges women face in postpartum periods. Priority should be given to initiatives that not only enhance immediate care during pregnancy but also sustain quality care that extends into the postpartum period. This comprehensive infrastructure can significantly help in reducing maternal mortality rates and ensuring that all mothers receive the care they deserve.
Innovative Solutions for Maternal Health
Exploring innovative solutions in maternal health care can play a significant role in reducing rates of pregnancy-related deaths. Technologies like telemedicine can bridge gaps in care, especially for women residing in rural or underserved regions. By providing remote monitoring and consultations, healthcare providers can better track maternal health throughout the entirety of pregnancy and into the postpartum phase. This ensures that women receive timely interventions and support, which is particularly vital for those at higher risk of complications.
In addition to technology, addressing social determinants of health is essential for improving maternal health outcomes. Programs focused on education, nutrition, and mental health support can foster healthier pregnancies and empower women with the resources they need. Incorporating community input in designing these solutions ensures they are practical and address the specific needs faced by various populations, thus enhancing overall effectiveness and outcomes.
Community Engagement and Maternal Health
Community engagement plays a pivotal role in enhancing maternal health outcomes. By actively involving local communities in health promotion initiatives, authorities can create culturally relevant programs that resonate with the populations they serve. This helps to build trust, improve health literacy, and ultimately empower women to make informed decisions regarding their maternal health. Community-based organizations can become essential allies in supporting mothers throughout pregnancy and into motherhood, ensuring that they have access to the resources and information needed to thrive.
Furthermore, involving community members in policy-making processes can foster a more responsive healthcare system that addresses the specific challenges faced by diverse groups. Advocating for maternal health rights and equity at the community level can help dismantle barriers to care. This grassroots involvement can lead to better-informed policies and a collective responsibility to care for mothers, significantly enhancing maternal health outcomes.
The Urgent Call for Policy Change
Addressing maternal mortality requires an urgent call for change at multiple levels of government. Policymakers must prioritize maternal health by allocating necessary funds and resources to ensure that comprehensive healthcare services are available for every birthing individual. Disparities in maternal care across different states showcase the need for a coordinated approach that standardizes quality care regardless of location or socioeconomic status. Policy reform must focus not only on improving healthcare access but also on implementing preventative strategies to reduce pregnancy-related deaths.
Moreover, advocating for policies that support mental health services and other social determinants of health is critical in shaping better maternal health outcomes. By ensuring access to mental health care, nutritional support, and community resources, we can lay the foundation for healthier pregnancies. It is essential to engage stakeholders from various sectors, including healthcare providers, policymakers, and community organizations, to create a holistic approach that addresses the multifaceted nature of maternal health.
Frequently Asked Questions
What are the primary causes of maternal mortality in the U.S.?
Maternal mortality in the U.S. is primarily caused by cardiovascular disease, with significant contributions from complications like hypertension, hemorrhage, and infection. Research indicates that many of these deaths are preventable, highlighting a critical need for improved prenatal care and postpartum support.
How do California’s maternal mortality rates compare to those in other states?
California has significantly lower maternal mortality rates compared to many other states. This variance suggests that systematic approaches to maternal health care in California could serve as a model for other states striving to reduce preventable pregnancy deaths. By analyzing what California does effectively, other states can implement similar strategies to improve maternal health outcomes.
What role do racial disparities play in maternal mortality rates?
Racial disparities are a significant factor in maternal mortality rates, with minority groups experiencing much higher rates of pregnancy-related deaths. For instance, American Indian and Alaska Native women face the highest mortality rates, underscoring the urgent need for targeted interventions to address these inequities in maternal health care.
Why is postpartum care crucial in preventing maternal mortality?
Postpartum care is crucial because maternal health issues can arise well after the initial weeks following childbirth. Late maternal deaths, which occur between 42 days and one year post-pregnancy, represent almost a third of all maternal deaths in the U.S. Therefore, enhancing postpartum support is essential to reduce the risks of preventable pregnancy deaths.
How does the U.S. maternal health crisis compare to other high-income countries?
The U.S. faces a maternal health crisis, leading high-income countries in maternal mortality rates. Many contributing factors include disparities in health care access, socioeconomic inequalities, and systemic biases within the healthcare system. Addressing these issues is critical for improving maternal health outcomes.
What systemic changes are necessary to improve maternal health and reduce mortality?
To improve maternal health and reduce mortality rates, a multifaceted approach is essential. This includes investing in public health infrastructure, enhancing access to quality prenatal and postpartum care, addressing healthcare disparities, and implementing policies that support maternal health across diverse communities.
What impact did the COVID-19 pandemic have on maternal mortality rates?
The COVID-19 pandemic has exacerbated existing maternal health issues, contributing to an increase in maternal mortality rates between 2018 and 2022. The pandemic highlighted deficiencies in the healthcare system, emphasizing the importance of providing continuous, high-quality maternal care during crises and beyond.
How can tracking maternal deaths improve maternal health outcomes?
Implementing effective tracking of maternal deaths allows healthcare providers and policymakers to understand trends, identify causes, and develop targeted interventions. Since a national system for tracking maternal mortality was only recently established, the availability of consistent data is crucial for informed decision-making to lessen the risk of preventable pregnancy deaths.
What are the implications of chronic medical conditions on maternal mortality?
Chronic conditions such as hypertension are increasingly affecting women of reproductive age, contributing to higher maternal mortality rates. It is vital to focus on managing these health issues before and during pregnancy, as they can significantly impact overall maternal health and outcomes.
| Key Points |
|---|
| In the U.S., more than 80% of pregnancy-related deaths are preventable. |
| The U.S. has the highest maternal mortality rate among high-income countries, continuing to rise between 2018 and 2022. |
| American Indian and Alaska Native women face the highest maternal mortality rates, at 106.3 deaths per 100,000 live births. |
| The leading cause of pregnancy-related death is cardiovascular disease, accounting for over 20% of deaths. |
| Late maternal deaths (42 days to 1 year postpartum) account for nearly one-third of total maternal deaths, highlighting the need for extended postpartum care. |
| State-by-state variation in maternal mortality rates indicates that some states perform significantly better than others, suggesting a need for policy improvements. |
| Investment in public health infrastructure and innovative care solutions is critical to reducing maternal mortality rates moving forward. |
Summary
Maternal mortality remains a pressing issue in the United States, with the country leading high-income nations in pregnancy-related deaths. Despite the fact that over 80% of these deaths are preventable, the maternal mortality rate has continued to rise from 2018 to 2022, reflecting significant disparities among different racial and ethnic groups. Efforts must be targeted towards enhancing prenatal and postpartum care, as well as addressing systemic inequities within the healthcare system. With collaborative actions and persistent investments in healthcare infrastructure, it is possible to transform these alarming statistics and improve maternal health outcomes for all women.